Da Nang Mission, June 2018
36 patients were assessed by the 2018 FTW team in collaboration with the Da Nang General Hospital doctors, and the week’s operating schedule was planned. The UK team was made up of representatives of the following specialities: General Surgery, Paediatric Anaesthesiology, Ophthalmic & Oculoplastic Surgery, Plastic Surgery, and Theatre Nursing. Patients were selected on the basis of the training and support levels required by the local team.
Cases included:
- nasal reconstruction
- craniofacial microsomia
- extensive congenital facial naevi
- juvenile hyaline fibromatosis
- eyelid grafting
- ptosis (droopy eyelid) correction
- burn scar release
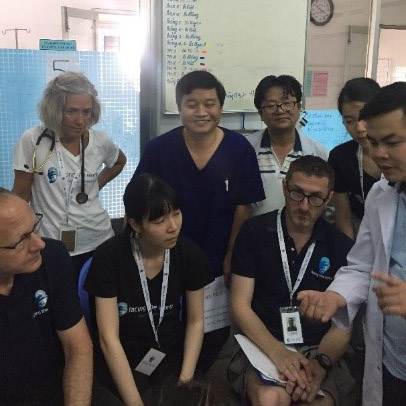


In collaboration with local surgeons, FTW operated on 12 patients over the four days. These cases included soft tissue reconstruction of facial asymmetry in craniofacial microsomia, a condition usually involving reduced volume of one side of the face including the external ear, cheek, jaws and mouth.
Extensive pigmented naevi are large pigmented areas of the skin and underlying tissues that are often in visible areas of the face and neck and have a dramatic appearance. The team of surgeons managed these cases with a combination of tissue expanders as a first stage, and, as a second stage, skin flaps to cover the areas when removed.
Juvenile hyaline fibromatosis is a rare condition in which children develop painful lumps under the skin and around the joints leading to contractures (permanent shortening). They also suffer from overgrowth of the gums. Administering a general anaesthetic in these children can be very challenging as they have short stature and limited mobility, and this case was managed by a combination of the local and visiting anaesthesiologists to successfully facilitate safe surgery.
The ophthalmic and oculoplastic team worked with the local surgeons on congenital ptosis cases, a condition where the upper eyelid does not fully open, and vision can be affected if not treated with specialist oculoplastic techniques.
Burns scar release was performed in the neck area and around the mouth and eyelids using skin grafts and skin flaps.

Reconstructions of each case were used as teaching examples, and patients from previous years were reviewed with the same teaching aims.
MRI and CT scans were provided by the hospital and sent to specialist radiologists in the UK for review and immediate reporting, so that these were discussed and also used for teaching.
The week was considered a great success by all the medics involved.